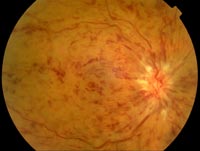
Central Retinal Vein Occlusion
 What's going on?
What's going on?
The central retinal vein has become occluded, resulting in back pressure and rupture of the veins throughout the retina. Arterial blood cannot enter the eye, the retina becomes ischaemic and part of it dies. The degree of ischaemia usually correlates well with the degree of visual loss. If the halt to blood flow is temporary, the vision may be fairly well preserved. With time the venous outflow returns, but the retinal ischaemia may persist. If the ischaemia is severe, the macula will be oedematous and neovascularisation may occur in the iris in response to release of vasoproliferative mediators. The new vessels on the iris may clog the drainage angle of the eye and cause rubeotic glaucoma. This can happen very quickly, typically within the first three months after the vein occlusion.
If I examine the patient, what will I find?
There will be extensive haemorrhages throughout the retina. The disc may be swollen and there may be an RAPD. Vision will be reduced.
What if I've diagnosed it?
Refer soon.
What will the hospital do?
The patient will be monitored for glaucoma and for resolution of the retinal haemorrhages and oedema. If new vessels develop, the patient will have aggressive argon laser pan-retinal photocoagulation to remove the dead retina cells and stop the ischaemic process.
What do I need to do?
Check blood pressure. Consider aspirin as a prophylactic measure.
What to tell the patient
They have sustained severe damage to the eye. The visual prognosis is variable and the best indicator of final vision is the vision immediately after the event. Intuitively, if they have very poor vision immediately after the vein occlusion they will probably not do well.
Problems that may arise, and how to deal with them
If the eye becomes red and painful, the patient may have developed rubeotic glaucoma. Feel the eye – if it is rock-solid, the patient probably has markedly raised pressure and should be seen by the ophthalmologist soon.

